Ugh! They did something similar with CPAPs too. Now you Rent to Buy because they found people were scamming they system to get free equipment to resell or got equipment that they never used.
So, what happens to the likes of Dash pods or other non-permanent pumps? What happens to CGMs that get used with a phone app vice a PDM, do they cease to exist? Seems like a great way to stifle innovation and ideas that don’t fit CMSs thought process…which doesn’t seem to involve much thought! Seems the bean counters have assumed control!
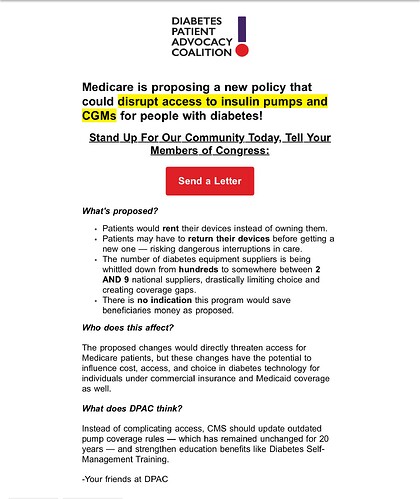
This is marketing spam from self-interested organisations. The proposed CMS change can be summarised as requiring the CMS to pay for pumps (Part B pumps) on a rental basis, as, indeed, they do for many assistive devices.
The reasoning is good; the CMS realised that the 5 year tie-in on a purchased pump really doesn’t work in a world where pump tech is changing so rapidly. Nothing changes so far as patient care is concerned; pumps are still provided on Part B under exactly the same rules, however the provider has to rent them out.
In fact this is an enormous benefit for those who are on Part B but cannot afford a Plan C or Plan G supplemental; those guys have to pay 20% of the pump cost up front, and the pump cost is massive. Someone who cannot afford Plan C or Plan G can’t afford that either. With Rental that all changes; pumps for everyone.
The dudes who are opposing this are the dudes who are making loads-a-money from the 5 year tie in. It’s the same as purchasing a new car on the never-never; you take out a loan to buy the best pump in the world then spend the next three years paying it back while it turns into the pump equivalent of an El Camino.
Y’all have lost your ability to comment; the comment period closed on August 29. I didn’t comment because I perceived that the result of this deliberation depended not on any comments but on how much money was paid to the current government. It is clear that the CMS knew what they were doing and had seen the problem and proposed a reasonable solution. I seriously doubt that this will make the slightest difference in the current political environment.
It’s Part B pumps.
CGMs have the same problem. I started on Medicare using G7. I’m tied to that for 5 years. I just got an Abbott Lingo to see if I could get better results from that but if I do I have to wait until 2030 to swap to the corresponding Abbott product. Duh
Here’s the link for the PDF, search it for “CGM”:
Here’s the relevant text for both Part B pumps and CGMs:
We also believe that classifying CGMs
and insulin pumps as items requiring
frequent and substantial servicing,
which would pay on a monthly rental
basis in accordance section 1834(a)(3) of
the Act under the fee schedule payment
rules and under the DMEPOS CBP in
accordance with regulations at 42 CFR
414.408(h)(8) and (j)(2)(iii), would have
the additional benefit of allowing
greater access to the latest technology
equipment. This would eliminate
beneficiary-ownership of the CGMs or
insulin pumps for new patients but
allow flexibility to switch to newer
technology equipment and supplies
more often than once every 5 years. The
beneficiary would no longer be locked
into the same CGM device or insulin
pump technology for 5 years. Moreover,
this would prevent the concerning
scenario where beneficiaries rely on
CGM or insulin pump technology that
has lost manufacturer support, resulting
in reduced software updates,
discontinued security patches, or
obsolete components. Such outdated
technology poses significant risks to
patient safety, data security, and
therapeutic efficacy. By reclassifying
these devices under the frequent and
substantial servicing payment class,
Medicare would ensure beneficiaries
maintain access to current, fully
supported technology that meets
evolving safety and performance
standards, which could ultimately
reduce the potential for outdated device
complications.
A simple logical argument that costs some Dudes loads-a-money so at this moment they are paying, paying, paying the best government that money can buy to get rid of this inconvenience to their frail wallets.
Diving into that govinfo doc…The acronym DMEPOS caused my inner 12 year old to giggle and it pops up all over the pages so I could not get very far in the excessively detailed document.
I did not discover whether Omnipod will continue under Part D pharmacy or if we on Medicare will have to switch to a DME provider. (If anybody can figure that out please let us all know, it makes a big difference with Part D open enrollment happening soon).
There’s a lot of discussion of Class 2 vs Class 3 devices (for example page 132). So I checked Google and found out that Omnipod 5 and Dash, and Dexcom G7, G6, Libre 3 and Eversense are all Class 2. Not sure what the importance of that is but they are all classified the same for the purposes of this document.
Anyway, I hope Edwards makes the cut as one of the approved DME providers. I have enjoyed their outstanding service since starting on Medicare and I do not like the idea of having to switch to a POS provider.
@jbowler Thanks for the info, what you say sounds good if accurate (not questioning you, but I’m a simple guy that doesn’t speak CMS sentences longer than 20 words). Wouldn’t it be great if they could actually write English that makes sense to the common man?! I know, I know, we’re trying to get government to talk with “the people of the land, the common clay of the new west…you know….” people like me!
I’ll re-read and try to interpret again…
Omnipods are not “Durable”; “DME” means “Durable Medical Equipment” and 3 days does not count. The problem arose first with the Eros pods; these had a durable component, the Omnipod Eros PDM, but for reasons that I’ve never seen explained (I suspect skullduggery) the CMS would not create a code for the Eros pods.
The eventual Insulet solution seems to have been the Dash pods. The Dash controller is a freebie and the Dash pod is therefore pretty much identical to an insulin pen, just some electrics and different cogs. Durable (reusable) insulin pens are covered under Part D so it makes a certain amount of sense for Dash and O5 pods to be covered under Part D.
The acronym DMEPOS is explained here:
As you can see an Omnipod (all varieties) is a “prosthetic device” when used by a T1, just like an ostomy bag. All insulin pumps are just like ostomy bags when used by a T1, i.e. they all replace the (necessary) functionality of an internal organ. So the CMS could have Part B’ed them on that basis but then the same applies to an insulin syringe when a T1 uses it. In that case the insulin should remain on Part D because neither prosthetic is DME.
See how complicated things can be made?
There’s no suggestion in there of any changes to coding. This comes down to numbers; the CMS has a big ledger of numbers and everything has to have a number. The Eros pods did not have a number so they weren’t covered by Medicare/Medicaid. The changes suggested seem to be changes to the treatment of things billed under the particular number that corresponds to durable insulin pumps.
Now if someone were to develop a CGM sensor that did not have a durable receiver then they would need a new code and be on Part D. Or not; test strips are on Part B because they are supplies for an incredibly expensive and long lasting piece of kit called a fingerstick meter, normally given away free like the Dash controller.
The only way to make sense of it is to look at the numbers, the billing codes, and use those to map back through the regulations; I’m just trying to summarise here! We’re all used to billing codes in the US but I was someone gobsmacked when I arrived here to find that every doctor’s office had to have a billing code specialist. Doc Martin never had one of those (the series is pretty accurate about what English GPs were like when I was growing up).
(c) John Bowler