well i havent paid anything yet, but i was supposed to pay around$520 ish
So that’s $1,040 total for three months (50% DME benefit) or $350 per month. That’s pretty good as a price, given that I ended up paying EdgePark $531 (I pay 100%). $350 is close to what I believe is the real price of 10 UST400 pods (1 box). That’s consistent with what I would expect from an employer plan where the employer is self-insured; Anthem is probably just doing admin, the payouts come from your husbands employer.
So now you simply call Anthem, insurance card akimbo, and ask for someone in the pharmacy benefits department. You need to telephone and speak to a real, working, pharmacy benefits person; the online stuff is likely to be confusing and only apply to 2019, the customer service guys can’t do the pharmacy benefits stuff you need.
Ask whether the Omnipod is covered as a pharmacy benefit. You will need to work with whoever you are talking to in order to distinguish the UST400 and Dash pods. You need to ask about 2019 and 2020 because the formulary (the list of pharmacy benefits) changes every year, and Insulet seem to be pushing really hard to have everything done as a pharmacy benefit.
I think it is likely you will find that Anthem doesn’t handle UST400 Omnipods as a pharmacy benefit this year, but they might cover them next year. I couldn’t see anything in the CA formularly about Dash pods as of 10/22/2019 but I only looked in one Anthem Blue Cross formulary.
In any case the person you speak to should be able to find the entries if they are there and, if in doubt, you can telephone Insulet and ask for the formulary codes for both UST400 pods and Dash pods then go back to Anthem with those. That’s what I had to do with moda to be sure we were both talking about the same thing. If Anthem come up with a pharmacy benefit check the price very carefully for each year and each variety of Omnipod (UST400 and Dash). I suspect you may find the amount you pay is also $175 for a month (i.e. half of $350).
There is one other way of doing it; get your doctor to write a paper prescription and take it to CVS or any of the pharmacies on the Insulet list; not Walmart, as of yet, and Walgreens turned out to be a bit tricky, although I use them now. The pharmacy will deduce the magic code number and then find out how benefits are available. If it is only through DME they will tell you they need to use their specialty pharmacy or that they can’t do it.
If you don’t get anywhere contact Insulet:
https://www.myomnipod.com/become-a-podder/insurance-coverage/pharmacy
That’s how I got the original email.
So I don’t have diabetes, I have adrenal insufficiency and I have been using an Omnipod loaded with cortisone instead-works wonderfully. It is covered under medical as DME and I pay 20% (approximately $58/box). I finally got approved for the Omnipod Dash through pharmacy coverage because I need a basal rate > 3u/hr for several hours, and the older OmniPod doesn’t support a basal >3u/hr.
Since this is pharmacy coverage, does anyone know how the copay works, is it like tier 1, 2, 3? Or is it a % like DME?
Most people find that items covered under pharmacy are cheaper than the DME %'s. With that said, there is so much variation in pharmacy coverage, I would say it depends.
Not sure why you are saying that.
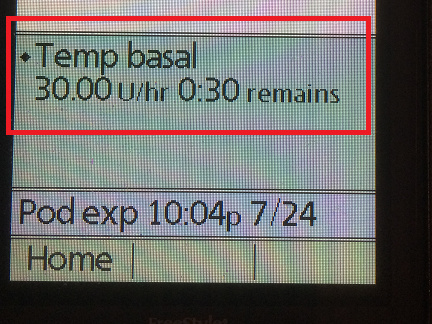
The old PDM supports basal rates of up to 30 units per hour. It can be via either a temp basal or a regular basal.
I just setup a temp basal to show it:
Now I’m really stumped. I went to settings—basal programs—and 3u is as high as mine will let me go. See pics of trying to add a new one. I tried for temp too. Since September of last year I’ve been trying to increase a few hours to 4u/hour and no dice, called Omnipod and they said I had to get the new Omnipod dash. They were not surprised by that limitation. I’ve been in the insurance process since then for pharmacy approval and because I have an off label use for it, had a few more hoops to go through. I’ve had this pdm for only a year because my last one was draining batteries really quickly so they replaced it. It was only in September that I tried to increase beyond 3u/hour per the recommendation of my docs and the fun with the insurance began… now I await my new Omnipod Dash.
Raj

Raj Samtani
+1.206.265.1318
Try this.
Go to:
Home>>Settings>>System setup>>Bolus/basal/calcs
The bottom item on that “Bolus/basal/calcs” page is Max basal
Change the max basal setting there before trying to create the basal profile.
Thank you for pointing that out!! I went on google and found the setting:
I went through all this trying to get the new one and I could’ve changed it all along. I called them and everything. This was the one and only justification on my insurance appeal that was approved approved today, oh well…LOL…maybe it’ll be cheaper supplies and I’ll get a fancy touch screen device to control it.
Well, now you can try them both and see which you like better! Good luck to you!
we have BCBS and they did not cover dash. ended up fine cause we decided to do omni poop instead which takes older eros pods anyway, which are covered. I was told ours did not because it falls under pharmacy benefit and not DME like usual and only certain pharmacies ship dash.
