While that’s true, there’s no reason to jump to the conclusion that hypoglycemia is the cause either.
The study that @oni posted yesterday regarding high CVD at lower A1c values in non-D people (not known at least) was suggesting that there may be some other factor (aside from hypoglycemia) that’s influencing the CVD risk of people with low A1c values. I would be interested to know what that might be.
Or maybe their RBCS just die quicker?
I think the frustrating part is that there really isn’t much data to guide here. i.e. we can all agree <7 is good. But until there is a follow-up study that allows the folks using the modern tools to be studied in a large group that includes the lower A1c people, I don’t think we will know the answer. Hopefully one of the Nordic countries will do an analysis.
Do you think that their RBCs dying quicker (assuming they did) might be contributing to their CVD risk? That’s an interesting idea.
My meaning isn’t necessarily hypoglycemia (although I personally, from everything I’ve read, think it is bad), but that diseases causing low-er BGs could confound the analysis.
For example, a few years ago there was a study that said people who slept a long time (or too little) had a very high mortality risk.
Yet, did the extra sleep really cause this, or was the analysis confounded by those who sleep because of disease, infirmity, depression, and just being bedridden?
If that is the case, it shouldn’t discourage people with D from lowering their A1c to 5-6% though.
I suppose that’s where I get a little lost in this whole thread.
In order for us to determine which A1c levels to target, we would need to understand the mechanism that is driving the CVD risk in the lower A1cs (in certain studies).
If it’s something entirely unrelated to diabetes, then there’s absolutely nothing wrong with targeting a low A1c and reducing our risk of complications.
haha don’t get me started on my favorite pet theory – that sleeping too much is bad!! I personally think it’s the sleep that does it, not some underlying condition 
As for the RBCs, I think my husband read that people’s RBCs last longer if they’re not exposed to excess glycemia, which shortens their life – which means the correlation between A1C and eAG gets a little fuzzier the lower down you go. Anyways, if excess glycemia can shorten RBC lifetime, I don’t see why other underlying health conditions or issues couldn’t do the same.
unless there is a risk specifically associated with the A1C being that low. Which we don’t know. And also because targeting a 5 something is, in my opinion, a lot harder and a lot more work, and requires a lot more time being low, than targeting a 6, for instance. Maybe not for everyone on this blog but for most people.
Agreed. I do think targeting a 5 is unhealthy if it requires someone to spend too much time hypoglycemic. I do not think this is true of everyone though.
I think there’s a difference between saying we shouldn’t target a 5 because the amount of work is not worth the benefit vs. targeting a 5 is unhealthy because of a higher risk of CVD.
As for erythrocyte death & low A1C, I guess we’d be talking about anemias, iron problems, sickle cell, hypertension, internal bleeding, liver disease, etc…
Apologies if some of these have been shared already:
This study of 13,000 people in US, not Japan, had a suspiciously similar chart for mortality of <5.5% a1c
https://www.nejm.org/doi/full/10.1056/NEJMoa0908359
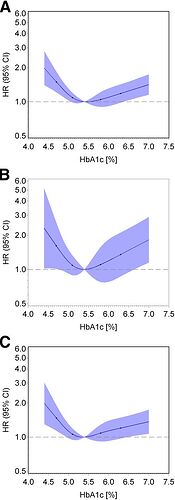
Confirming this, a large study in Germany showed a U-shaped curve of mortality as well:
http://care.diabetesjournals.org/content/38/2/249.full
What’s interesting about this curve to me is how much more quickly your mortality risk goes up on the low side than the high!
http://care.diabetesjournals.org/content/34/12/2548
A U-shaped association was found between continuous HbA1c and all-cause mortality, with the lowest risk at HbA1c levels of 5.4–5.6% (36–38 mmol/mol) and a significantly increased risk at HbA1c levels ≤5.0% (≤ 31 mmol/mol) and ≥6.4% (≥46 mmol/mol).
However, a meta-analysis of these studies seems to have a flat curve below 5.7%.
https://www.nature.com/articles/srep24071
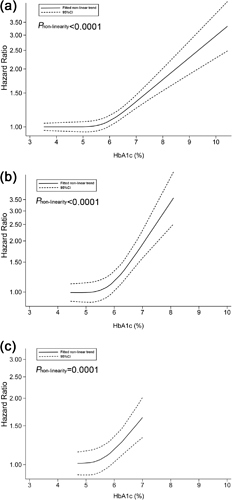
The newest meta-analysis, actually, is more of our holy grail. It splits recommendations for diabetics and non-diabetics. But its conclusion is surprising.
our data suggest that clinicians should advise their patients with diabetes to maintain their HbA1c levels in the range of 6.0% to 8.0% and also that the target limits for HbA1c in individuals without diabetes should be in the range of 5.0% to 6.0%.
Not sure anything more on this topic will be released for another year or more. The only thing relevant to cite it is another meta-analysis showing weight training may lower your A1c between 0.3-1.3%
https://doi.org/10.1007/s40279-018-0861-0
So that paper is somewhat of a final word, tentatively.
If <5.4% is more deadly, these articles suggest some possible reasons:
If I had to guess why this chart looks so odd (diabetics are healthier btw 7-8% than 6-7%!) is that hypoglycemia-related deaths start going up slowly under 7%, and since children die from it, it skews the results away from the long-term illnesses.
And anemia, liver disease, etc. diseases only show effects for non-diabetics closer to 5% (unlikely they are also dying from hypoglycemia complications between 5-6%!)
And I don’t think the hazard ratios are standardized to a combined population, else diabetics 6-8% would be healthier than the general pop!
Just a guess.
Thanks for posting these.
My takeaway is that if your A1c drops below 5.4%, then it may be best to evaluate your overall health and determine what mechanism is enabling you to obtain an A1c in that range. If that’s frequent hypoglycemia, then some adjustments should be made.
If it’s not frequent hypoglycemia, then insisting on tests to ensure that there aren’t other problems resulting in a low A1c is a good idea.
Based on what I’ve read in these studies, 5.4%-5.7% sounds like the ideal target range.
my understanding is that hypoglycemia-related deaths are still more common in older adults – especially older, insulin dependent T2s. While there are certainly many, many kids who experience hypoglycemic seizures, I don’t think we have great stats on how many people actually die from hypoglycemia (Dead in Bed is not strictly due to this, but rather may be caused by underlying autonomic dysfunction which could be in turn affected by hypoglycemia or something else).
I think it’s fair to say, though, that the relationship between hypos and tight A1C is not that straightforward; i’ve seen a number of studies where those with the poorest control (i.e. A1C >8) are at much higher risk for hypogycemia than those in the 6 to 7 range. I think that’s intuitive on some level; for us, almost all our lows occur after treating highs. We don’t just have lows out of nowhere; they’re reactive when you’re in the high range and you don’t know exactly how much insulin you need to bring down a high. So someone who is always roller-coastering between high and loiw is, in my opinion, much more likely to be at risk of hypogylcemia than someone between 6 and 7, who is likely much more tightly controlled.
I agree completely.
The slope of the meta-analysis (the most rigorous, high quality study type that exists on the scientific hierarchy) shows an obvious, but modest uptick in mortality rate for a1c below 7-8% in diabetics. If it isn’t hypoglycemic events skewing those numbers, then any idea what is affecting it? If it is something else, then we would be smart to figure it out and try to avoid it!
The authors do not discuss causes other than linking a meta-analysis on hypoglycemia risks.
(Don’t have access to this paper right now, but will try to get later.)
Not much to go on, but I think it would be unlikely that this trend was estimated incorrectly in almost every study we have thus shared and the studies these authors analyzed and compared.
Our findings show an increase in all-cause mortality when HbA1c levels are above 8.0%, but also below 6.0%, for people with known diabetes and above 6.0% or below 5.0% for clinical non-diabetic patients. Thus, our data reinforce previous findings[26] and support the clinical importance of preventing hypoglycaemia in the diabetic population and in those without a diagnosis of diabetes, in such a way that it suggests that the optimal range for HbA1c might be established from 6.0% to 8.0% in patients with diabetes and from 5.0% to 6.0% in non-diabetic patients. Although previous studies have reported an increase in mortality risk by each 1% increase in HbA1c, their estimates are based on the assumption of a linear relationship between these variables, which the data from studies included in this review did not show.
Given that we’re unable to view the study, I doubt anyone could provide any insight. Anything anyone says would simply be speculation.
I’m not able to view the study at all, and I do not see the paragraph above when I click on the link provided. Were you able to access it elsewhere?
I too lack access so perhaps not super productive to discuss just yet. But just looking at the sources they include, almost all the studies relate to T2Ds, so that’s one limitation right there. Another is that the vast majority of these studies are on hospitalized or critical-care patients, also with T2D. I also am not surprised that hypoglycemia could be associated with negative outcomes in that population as well, though not sure the direction of the causality. Another study included finds a link to hypoglycemia and mortality, but not “drug-induced” hypoglycemia and mortality (i.e. the ones driven by insulin or other diabetes drugs, I am presuming) – and those who had hypoglycemia tended to be older and have other comorbidities. A followup analysis of the ACCORD study also found that drug-driven hypoglycemia was not associated with increased mortality, whereas spontaneous hypoglycemia (i.e. not tied to the therapy) was. In general those who experienced hypoglycemia tended to be older and thinner and to have higher risk factors associated with adverse outcomes in a number f the trials.
And the few that focus on T1s (which are quite large, like DCCT and EuroDiab) do not seem to find an increased risk of CVD associated with hypoglycemia. So… I’m just not sure it’s productive to lump T2s and T1s together. It’s really quite possible that T2s have some separate underlying disease process which makes it better for them, all things considered, to maintain slightly higher A1Cs.
Also have to say I’m not sold on the idea of a meta-analysis being “the most rigorous, high-quality study type that exists on the scientific hierarchy.” Meta-analyses are extremely easy to do (you basically just need a search and institutional access to a variety of papers) and are a dime a dozen. Depending on how you select your inclusion criteria, you can wind up with very different results. So I think meta-analyses are interesting and useful somewhat, I would take the data from a well-designed, randomized, controlled trial with a large number of participants any day over a meta-analysis. Not to say they’re useless but I just think there are a lot of pitfalls when designing them.
Finally, that’s not to say that I don’t think it’s plausible that hypoglycemia adversely affects cardiovascular disease. The fact is that in the immediate aftermath of a hypo, there are lots of chemicals released that could promote a clot from breaking free and lots of pro-clotting factors released in the blood, among other things. Your BP is also transiently raised, etc. So I mean there’s certainly a very reasonable mechanism there.
I just think the jury is out on whether hypoglycemic events are worse for T1Ds than the negatives of running higher blood sugar. I’m not convinced there’s a strong benefit to running an A1C of 5.5, but neither am I convinced that someone who is T1 and experiences frequent hypoglycemia as a result of insulin therapy is at dramatically higher risk of dying early.
I found another research paper covering risks at low A1c levels. It had a list of possible conditions that can cause this, so I thought I’d post them here in case someone with a low A1c finds this thread and wants to ask their doctor about it. This way they’d at least have a list of possible causes.
RBC Lifespan ↓, HbA1c ↓
- Increased production (high altitude, pregnancy, erythropoietin use)
- Hemorrhage
- Chronic bleeding
- Hemolytic anemia
- Chronic kidney failure
- Liver cirrhosis, chronic hepatitis, ribavirin use
- Alcoholic liver disease
- Folic acid deficiency
- Hemoglobinopathies (eg, thalassemia major)
- Spherocytosis
- Aplastic anemia
“However, low or extremely low HbA1c (5.0% or 4.0%) may occur in apparently healthy individuals.”
What I have heard @Eric say over and over and over again is that low A1c in T1D is completely different from low A1c in non-T1D.
I trust Eric.
Bottom line.
I can add one to the list from personal experience.
Chemo treatments (which lowers RBC counts).
Had my lowest ever A1C, 4.6 during chemo, only time below 5.
How do you measure better?
Health improvements/longevity vs quality of life ?